The domain of male fertility is not limited to the mere analysis of sperm parameters or lifestyle adjustments; it's an intricate ecosystem that also extends to the realm of sexual health. One of the most overlooked but fundamentally critical elements is the role of sexually transmitted infections (STIs) in shaping—or misshaping—male fertility. This article delves into the pathological interplay between STIs and fertility, preventative strategies, the indispensable role of semen analysis, and how innovations like Sapyen are pioneering shifts in fertility management paradigms.
Article Highlights:
- Unpacking the complex relationship between STIs and their multifaceted negative impacts on male fertility.
- Articulating nuanced preventative methodologies to guard against STIs and their debilitating effects on reproductive health.
- The critical function of semen analysis in fertility assessment, bolstered by revolutionary technological advances.
- Profiling Sapyen as a game-changer in the arena of accessible, efficacious, and personalised fertility solutions.
The Cascading Consequences of STIs on Male Fertility: A Microscopic Battlefield
It's essential to comprehend that STIs such as chlamydia and gonorrhea don't merely cause discomfort or short-term symptoms; they engage in a form of cellular warfare that devastates the male reproductive system. The consequences can manifest as inflammation, fibrosis, and subsequent scarring, primarily targeting critical anatomical regions like the epididymis and vas deferens. This tissue damage presents as a physical roadblock, impeding the typical transport and maturation of sperm. Moreover, STIs can incite immunological responses that adversely affect testicular function, leading to decreased sperm quality and count.
A Proactive Framework for STI Prevention: Beyond Conventional Wisdom
Taking an active stance against STIs isn't merely a checklist but an ongoing exercise in strategic preparedness.
-
Holistic Safe Sex: This includes not just the habitual use of condoms but also the consideration of dental dams for oral sex, and proper sterilization techniques for sex toys, often overlooked vectors for STI transmission.
-
Routine, Comprehensive Screening: Beyond standard testing, insist on comprehensive panels that test for a wide range of STIs, especially if you engage in diverse sexual activities or have multiple partners.
-
A Culture of Open Communication: This is not limited to merely discussing STI status. It should be a broader dialogue about sexual history, prevention strategies, and mutual commitments towards periodic testing.
-
Targeted Vaccination: While vaccines for HPV and hepatitis B are commonly discussed, keep abreast of emerging vaccines and prophylactic treatments for STIs, and consult your healthcare provider for tailored recommendations.
The Relevance of Sapyen in Managing STI-Related Fertility Concerns
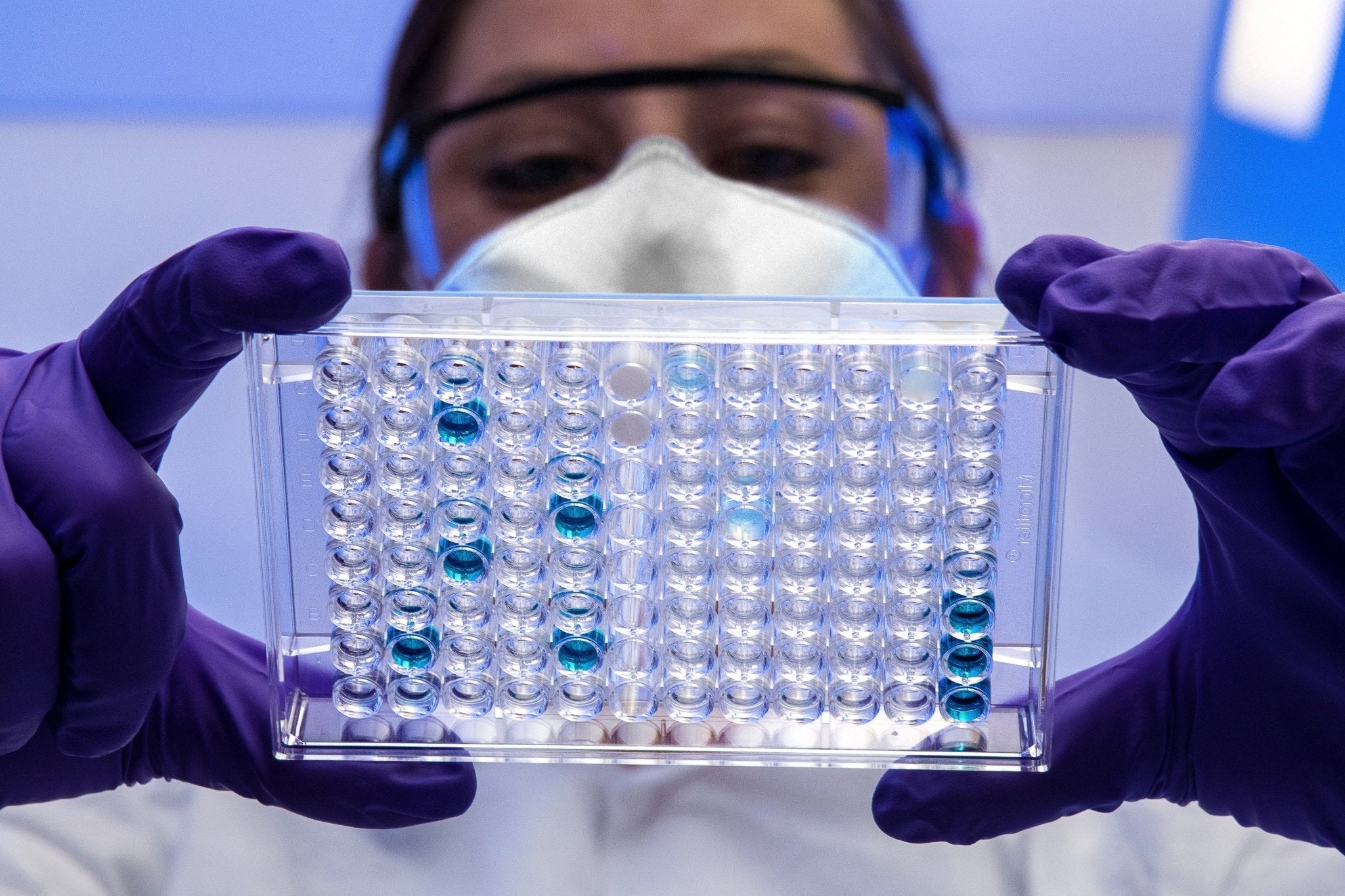
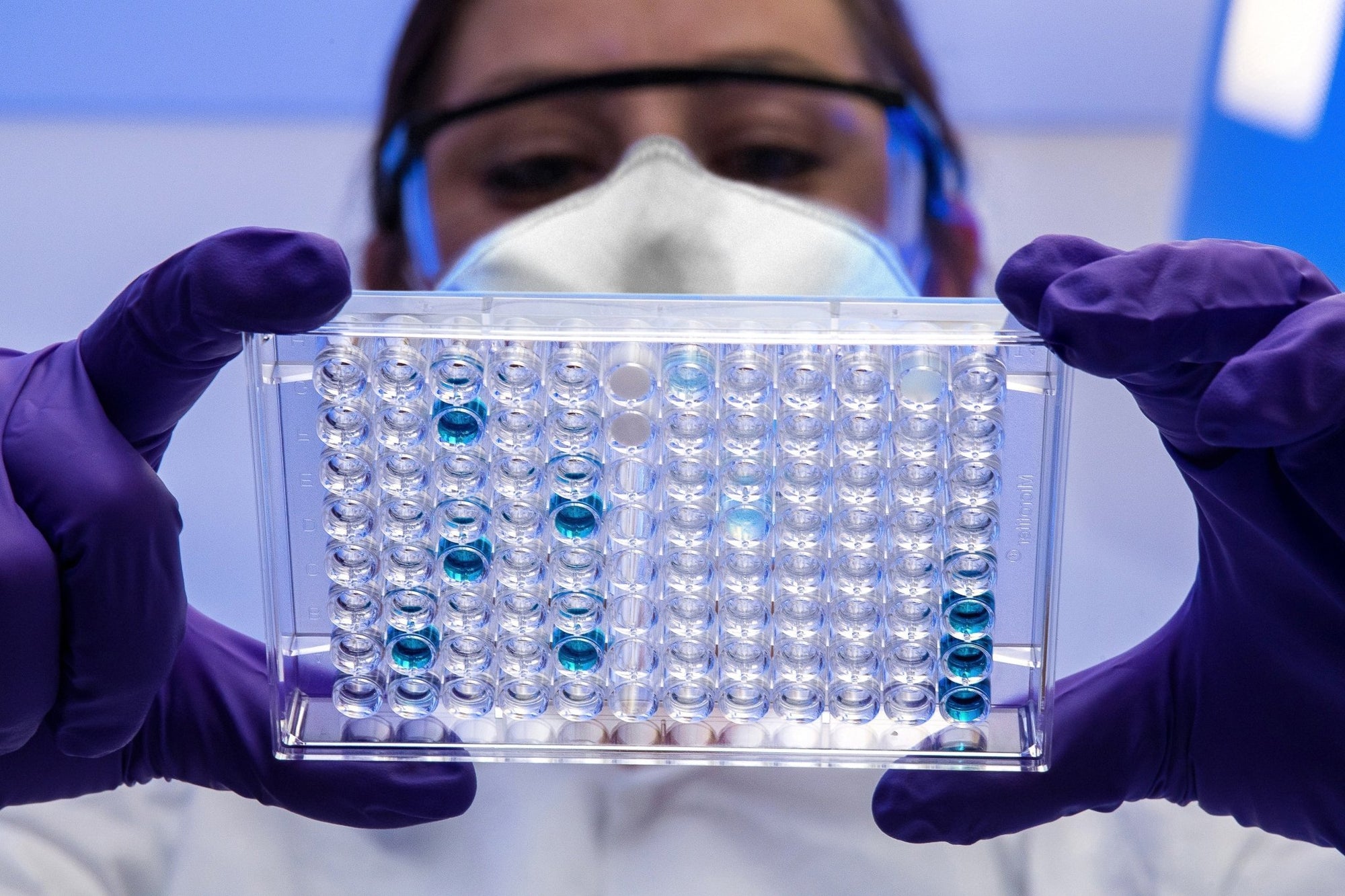
While the prevention of STIs is paramount for maintaining reproductive health, early detection and management are equally critical. For men concerned about how STIs may have impacted their fertility, timely evaluation through semen analysis is vital. That's where Sapyen steps in. We offer an innovative yet accessible way to assess fertility parameters potentially impacted by STIs—right from the comfort of your home. The proprietary transportation medium used by Sapyen ensures that even if you cannot immediately send off the sample, its integrity remains preserved for up to 72 hours. This dramatically expands the timeframe for a comprehensive and accurate analysis, aiding in quicker, more effective decision-making concerning your reproductive health.
This immediate feedback loop allows you to consult healthcare professionals with specific, actionable information, considerably expediting your path to appropriate medical intervention or family planning.
Conclusion: Architecting a Future of Informed Fertility
Navigating the labyrinthine complexities of STIs and male fertility is neither simple nor straightforward, but the instruments and strategies to mitigate risk and safeguard reproductive health are within reach. It involves implementing a nuanced, multi-layered approach to sexual health, regular testing, and a conscious choice of preventative methods. Additionally, advances in at-home semen analysis technology, epitomised by Sapyen, offer an unparalleled level of control and insight into one's fertility status. In synthesising these components, men can actively architect a future where fertility uncertainties are replaced by informed, empowered choices.
References:
- World Health Organization (WHO). (2016). Sexually transmitted infections (STIs): Fact sheet.
- Centers for Disease Control and Prevention (CDC). (2020). Condom effectiveness.
- Centers for Disease Control and Prevention (CDC). (2020). STDs & infertility.
- American Sexual Health Association (ASHA). (n.d.). Talking to your partner about STDs.
- Centers for Disease Control and Prevention (CDC). (2020). Vaccines & immunizations: HPV vaccine information for young adults.
- Practice Committee of American Society for Reproductive Medicine (2013). Diagnostic evaluation of the infertile male: a committee opinion. Fertility and Sterility 100(2), 294-301.
- World Health Organization (WHO). (2010). WHO laboratory manual for the examination and processing of human semen (5th ed.). Geneva: World Health Organization.
- Practice Committee of American Society for Reproductive Medicine in collaboration with Society for Male Reproduction and Urology (2015). The clinical utility of sperm DNA integrity testing: a guideline. Fertility and Sterility 103(3), e18-e27.
- Levine H., Jørgensen N., Martino-Andrade A., Mendiola J., Weksler-Derri D., Mindlis I., Pinotti R., Swan S.H.(2017) Temporal trends in sperm count: a systematic review and meta-regression analysis, Human Reproduction Update 23(6), 646-659.