The Negative Impact of STIs on Male Fertility
STIs pose a significant risk to male fertility, potentially leading...
Despite being highly effective, vasectomies aren't 100% guaranteed. A small percentage of cases result in incomplete sperm clearance or recanalization, where the severed vas deferens reconnects. This can lead to unintended pregnancies. The PVSA ensures that your vasectomy has fully succeeded by confirming the absence of sperm in your semen.
Directly after a vasectomy, there's still a possibility of sperm present in the upper portion of the vas deferens. It usually takes about 20 ejaculations to expel these remaining sperm. Conducting a PVSA three months post-vasectomy is essential to ascertain that your semen is completely sperm-free, significantly reducing the risk of an unplanned pregnancy.
The PVSA is a fundamental component of your long-term contraceptive planning. Knowing with certainty that your vasectomy is effective allows you to make informed decisions about your sexual and reproductive health. It removes the underlying worry of an unexpected pregnancy, making it a critical aspect of responsible family planning.
A PVSA provides more than medical confirmation; it also offers legal and emotional peace of mind. In legal contexts, such as divorce or custody cases, proving that you've undergone effective sterilisation can be pertinent. Emotionally, the confirmation from a PVSA can relieve concerns about accidental pregnancies, enhancing trust in the vasectomy's effectiveness.
Undergoing a PVSA post-vasectomy is a globally recognised medical protocol, not merely a suggestion. This step is strongly recommended by urologists and health organisations worldwide as a necessary conclusion to the vasectomy process. It's considered standard practice to ensure the procedure's success and the patient's well-being.
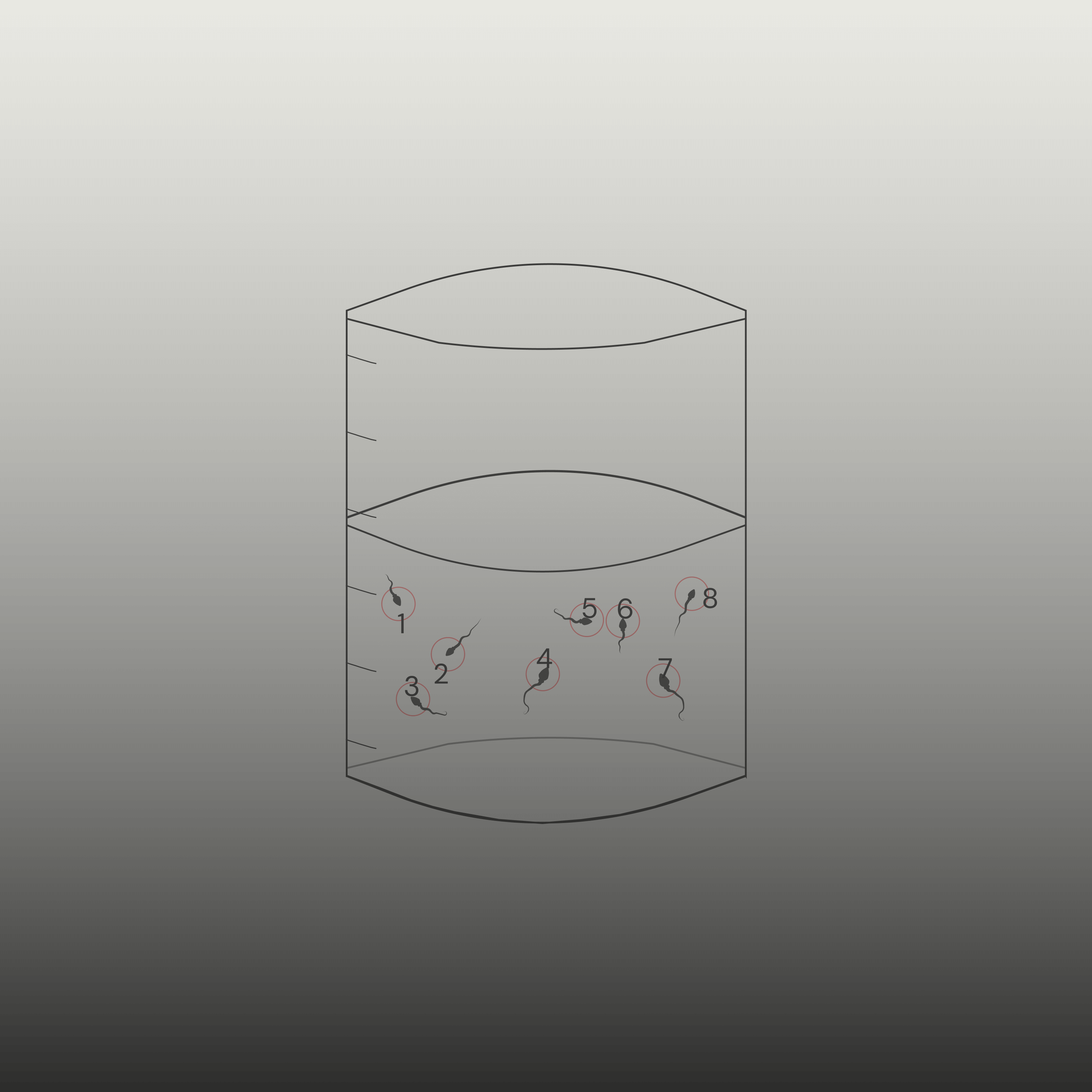
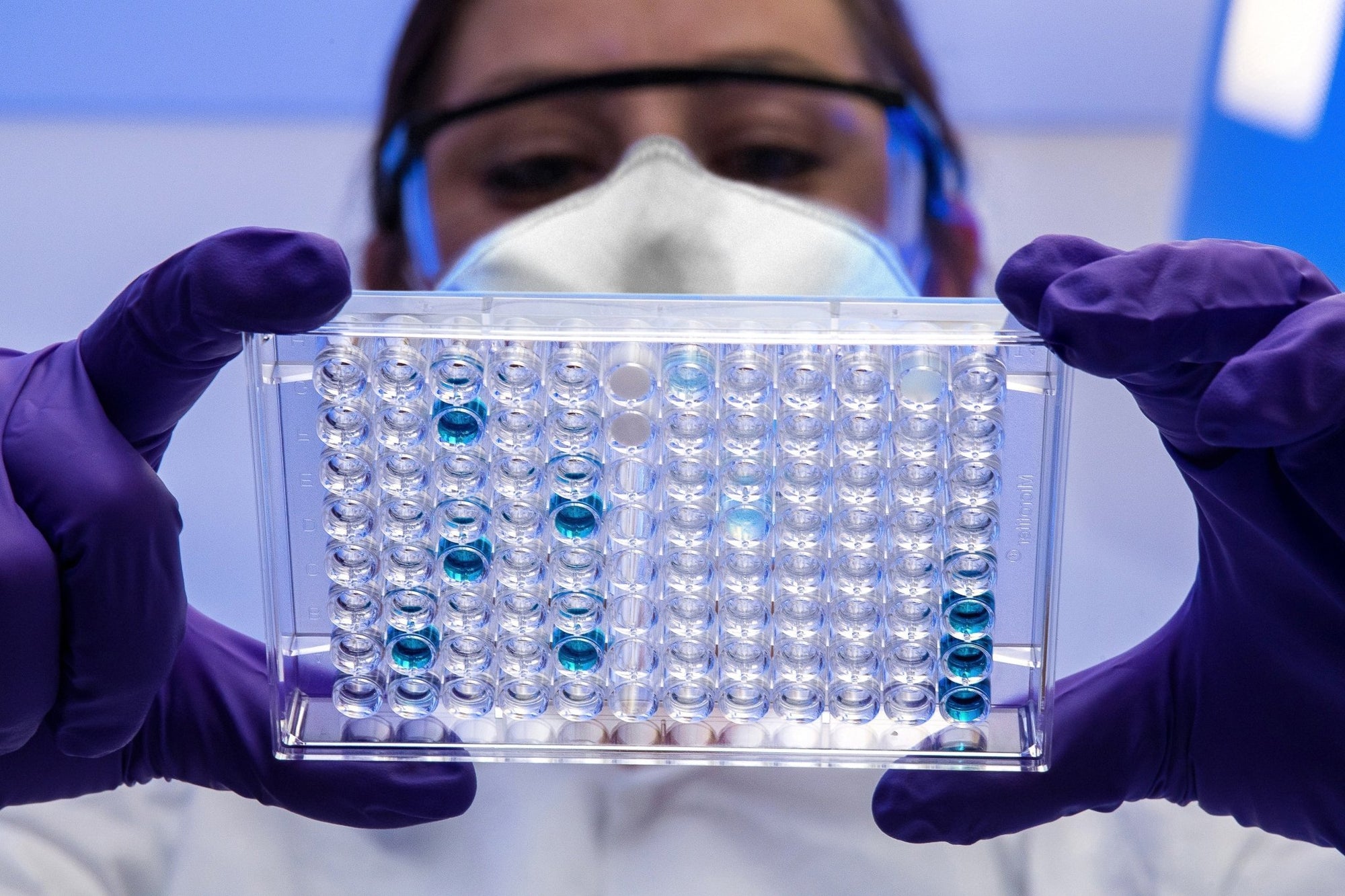
Utilising a meticulous approach, sperm are examined under 50 high-power fields. This intensive scrutiny is pivotal for determining the presence of sperm post-vasectomy. The absence or significant reduction of sperm count is a primary indicator of a successful vasectomy, ensuring a reliable measure of the procedure's effectiveness.
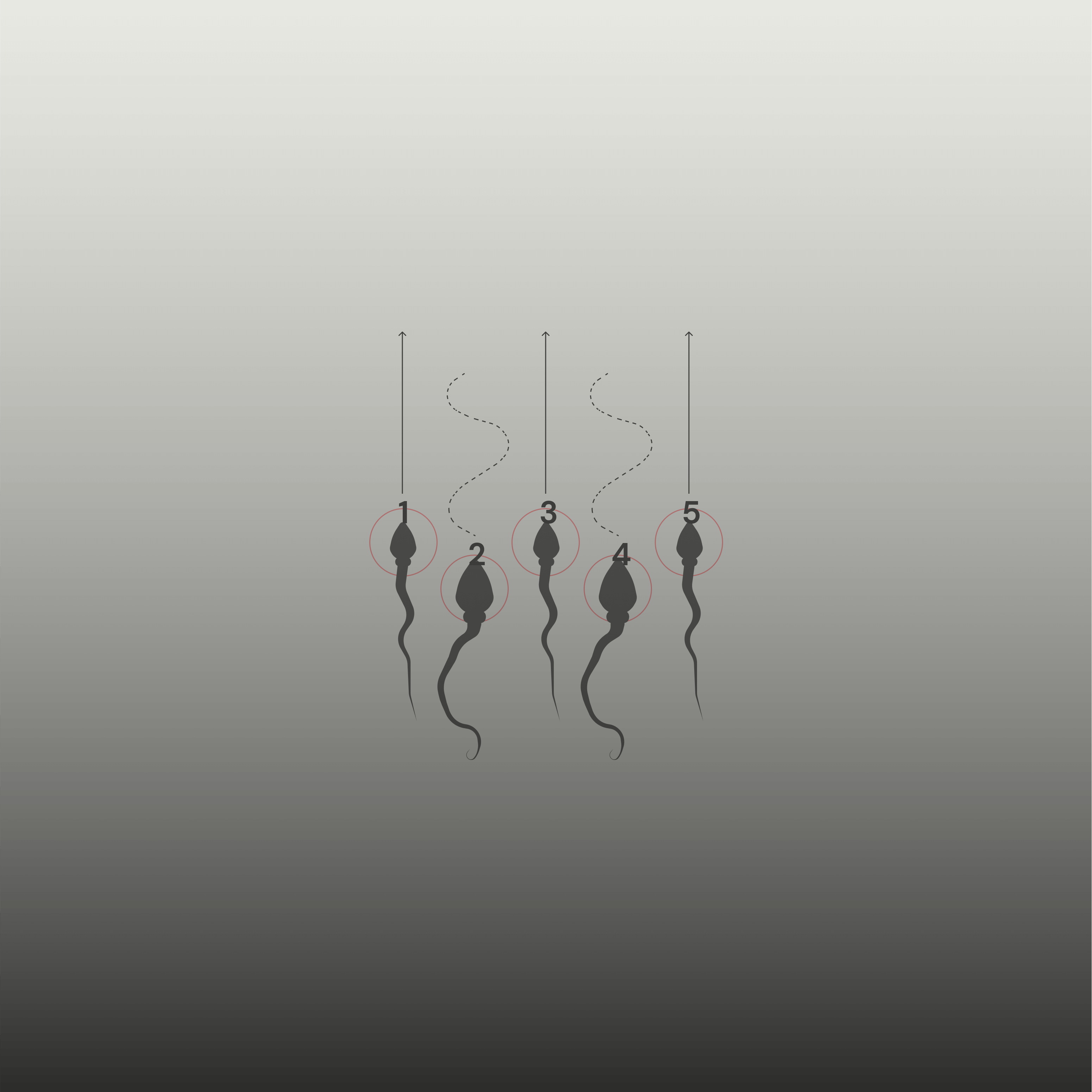
In the rare instances where sperm are detected, their motility is rigorously evaluated. The objective is to ascertain that any remaining sperm are non-motile, which is a critical factor post-vasectomy. Non-motile sperm, unable to swim or progress, may signify a successful vasectomy, as they lack the capability to fertilise an egg.
The volume of semen produced is measured, as it remains a relevant factor post-vasectomy. While the volume is not directly indicative of the success of the vasectomy, it provides insight into the normal functioning of the seminal vesicles and prostate, which are unaffected by the procedure.
STIs pose a significant risk to male fertility, potentially leading...

Explore the critical role of targeted nutrients and exercise regim...

In the complex landscape of fertility, men's age plays an underexpl...
Your Cart is Empty